Objective: Tumor protein p53 (TP53) is the most frequently mutated gene in cancer, and is associated with high-risk disease, resistance to conventional therapies and dismal outcomes. The characteristics and prognostic value of TP53 gene abnormalities in patients with myelodysplastic syndromes (MDS) need to be further clarified.
Methods: A retrospective analysis was conducted on 96 patients diagnosed with MDS accompanied by TP53 gene abnormalities at Fujian Medical University Union Hospital, from January 2017 to June 2023.
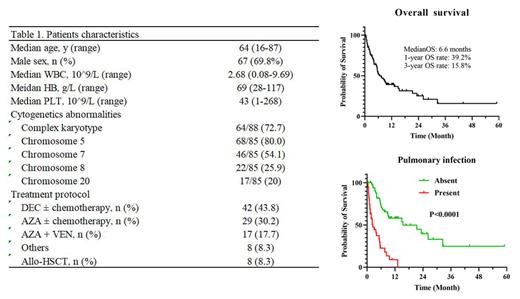
Results: Among these 96 patients, 88 cases had TP53 gene mutations and 8 cases had TP53 gene deletions. There were 67 male patients and 29 female patients, with a male-to-female ratio of 2.3:1. The age of the patients ranged from 16 to 87 years, with a median age of 64 years. Eighteen cases (18.7%) were MDS with low blasts, 29 cases (30.2%) had increased blasts-1 (IB-1), and 49 cases (51.1%) had increased blasts-2 (IB-2). Twenty-two patients (22.9%) transformed to acute myeloid leukemia (AML) during the disease course, with a median transformation time of 6.5 months. Chromosome karyotype were available for 88 patients, and complex karyotypes were noticed in 64 (72.7%) cases. Among the 85 patients with fluorescence in situ hybridization (FISH) results, the proportions of abnormalities in chromosomes 5, 7, 8, and 20 were 80.0%, 54.1%%, 25.9%, and 20.0%, respectively. MDS patients with TP53 gene abnormalities showed poor survival, with a median overall survival (OS) of 6.6 months, a 1-year OS rate of 39.2%, and a 3-year OS rate of 15.8%. Patients with pulmonary infection at the time of diagnosis presented extremely worse prognosis compared to those without pulmonary infection, with a median OS at 2.4 months and 15.4 months, respectively (P<0.0001). It should be noticed that 15 out of 17 (88.2%) patients with pulmonary infection presented immune dysfunction, with abnormal ratio of CD4-positive T lymphocytes to CD8-positive T lymphocytes. 29 patients received azacitidine-based treatment and 42 patients received decitabine-based treatment, the median OS were 5.9 months and 8.3 months, respectively (P=0.4446). Seventeen patients received a combination of azacitidine and venetoclax, with a median OS of 5.7 months, which did not improve the prognosis. Eight patients underwent allogeneic hematopoietic stem cell transplantation (Allo-HSCT), with a median OS of 15.2 months, compared to a median OS of 8.3 months for those who did not undergo Allo-HSCT with similar characteristics (P=0.9637).
Conclusion: TP53 gene abnormalities in patients with MDS are frequently accompanied by complex karyotypes and abnormalities in chromosomes 5, 7, 8, and 20. Currently, the prognosis of MDS patients with TP53 gene abnormalities remains poor, and treatment regimens based on demethylating agents have limited efficacy in this population. In combination with venetoclax or Allo-HSCT also can not improve survival. An abnormal ratio of CD4+ T lymphocytes to CD8+ T lymphocytes and pulmonary infection are an important adverse prognostic factors. In order to overcome the dismal survival of these population, further studies are still needed.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal